In this week’s edition of River City Data, I share a big update to the COVID tracking site, break down the latest numbers and trends (spoiler alert - I’m worried), go into the weeds on why we map rates and not counts, and share my interview with Dr. LJ Punch. - Chris
COVID-19 by the Numbers
Total cases in MO: 169,311 (+10,547 from last Friday)
7-day average of new cases per day in MO: 1,881.29 (-80.14 from last Friday)
Counties with the highest per capita rates of new cases per day this past week:
Osage (119.58 per 100,000), Pettis (77.21), Cole (72.79), Miller (70.15), Moniteau (69.83),
and Nodaway (65.26)
Total deaths in MO: 2,734 (+184 from last Friday)
7-day average of new deaths per day in MO: 29.00 (+16.57 from last Friday)
These numbers are current as of Thursday, October 22nd. Additional statistics, maps, and plots are available on my COVID-19 tracking site.
New on the COVID-19 Tracking Site
In the past week, I worked with my colleague Tim Wiemken to add a unique data set to the COVID-19 tracking site - nursing home cases and mortality. These are data that Missouri has refused to make public, but the federal government publishes every week.
Unfortunately, the federal data are tough to wade through. So, we’ve made a few interactive maps and tables to help identify facilities and counties that have been particularly hard hit by COVID-19. Tessa Weinberg, a reporter for the Missouri Independent, has an article out on this topic today. She summarizes findings from our initial look at the data and provides a reaction from Gov. Parson.
Several new data sets are still on the to-do list, including Illinois ZIP code data and some additional statewide and local demographic data.
Summary for the Week Ending October 23rd
There are two big things to discuss this week—first, the data issues. When I wrote last week, they had finally been resolved. However, I rely heavily on 7-day averages to “smooth” out day-to-day swings in the number of reported cases and deaths. This means that yesterday was really our first chance to see the virus’s state since the end of September. Let that sink in for a moment - October 22nd was the first chance to get a real sense of how transmission and mortality are progressing since last month. This all boils down to Missouri’s struggles to implement their new dashboard, which I discussed last week.
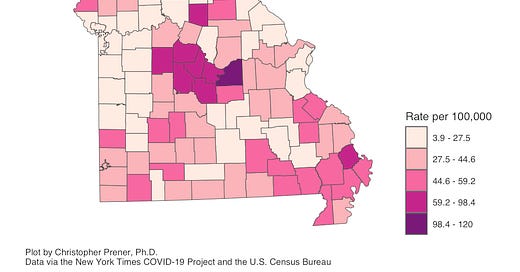
When the dust finally settled yesterday, we saw a broad swath of regions with high numbers of new cases. These include counties in southeastern, southwestern, Mid-, and northwestern Missouri with per capita 7-day averages that are several times higher than what we’re seeing in metro St. Louis and Kansas City:

Osage County has the highest 7-day averages right now, part of a concentration of new cases encompassing the Jefferson City and Columbia metropolitan areas and part of the Lake of the Ozarks region. This is a big part of the reason why the “outstate” 7-day averages remain relatively high right now:

“Outstate” makes up 56% of new daily cases currently, which is down a bit from the approximately 62% of new daily cases they had been at. Nonetheless, this represents a significant burden for smaller cities and rural areas throughout the state.
This gets me to the second big topic—one potential consequence of this is increasing pressure on hospitals. In the past ten days, we saw this unfold in at least four regions. In Springfield, Cox Health reported all-time high numbers of in-patients, and Mercy activated its mobile COVID emergency department. In the Lake of the Ozarks region, a third of the in-patients at Lake Regional Health System’s hospital were there for COVID-19 at one point. In Kansas City, eight hospitals went on diversion on Wednesday, 10/14, and five were on diversion the following night as well. “Diversion” refers to a situation where ambulances are not accepted for all but the most critical patients. And in St. Louis, Dr. Garza, the head of the local hospital task force, stressed that “all of our indicators are red.”
One of my biggest concerns with the pandemic are the consequences of hospitals getting overwhelmed. We’re at levels right now in St. Louis that are comparable to mid-May:

Why is this happening now? We have a couple of possible culprits. These include patients being transferred into St. Louis from more rural, outlying areas of the region. They also include patients hospitalized due to widespread transmission in counties that do not have mask requirements like St. Charles County. The 14-day averages for ZIP Code cases in St. Charles are deeply concerning:

My fear right now is that this is a dress rehearsal for where we might be in a few weeks - multiple hospitals around Missouri inundated with patients alongside rising transmission rates. I hope that it does not come to that, but as I said in the intro, I’m worried.
Into the Weeds
When you look through the maps on my website or above in tonight’s newsletter, you’ll notice that I always map rates: cases per 1,000 residents, deaths per 1,000 residents, cases per 100 beds in a nursing home, etc. This is an essential mapping rule - we always need a consistent baseline to compare the jurisdictions we’re mapping. In the new nursing home maps, a nursing home may have more cases simply because it is larger. So, instead of mapping those cases directly, we calculate a rate per 100 beds that provides a standardized way of comparing long-term care facilities of different sizes. Cartography wizard Ken Field has an excellent blog post on mapping COVID if you want to dig further into this!
Weekly Interview
This week’s interview is with LJ Punch, MD, who is a truma surgeon, Washington University in St. Louis Medical School professor, and an activist involved in addressing gun violence in St. Louis. You can learn more about their work in this recent TEDxGatewayArchSalon Talk and on the website for The T.
CP: What has it been like being a physician and treating patients with COVID-19?
LP: The primary feeling for me which came early in the pandemic was a sensation of drowning. It was clearly a disease with claws of an eagle, strength of a lion and teeth of a shark. There was a weird combination of symptoms that included a dense respiratory failure as well as a million tiny pulmonary embolisms, strokes and myocardial infarctions. It was surreal to have such a serious disease gripping a patient and to not have their families at the bedside to support them and also understand the severity of the illness. While as a surgeon I am used to working in masks and protective gear, the burden of every interaction requiring such immense precaution was challenging. Finally, not knowing if I was doing enough to avoid becoming a vector to infect others was very stressful, thankfully I avoided that.
CP: Something I’m particularly concerned about are disparities in who is getting sick and dying from COVID-19 in our St. Louis community. What disparities are you seeing personally? What worries you?
LP: I made a video on March 16th in which I discussed my concern that I knew the virus would follow patterns of transmission similar to violence in our city and that was due to the structural and social burdens that black and brown people carry here and across the country. I will forward it to you. I saw an ICU at Christian NE hospital which was 99% full of black folx and it was unreal. I saw people dying and had friends who had many family members sick with the disease. It was a flood and it was as if those who were already living in low country had no hope of survival. This was not particularly surprising to me for the reasons I share in that video, but it was still disturbing and sad. That is why I worked so diligently with PrepareSTL and have been part of campaign that has distributed over 150K masks and PPE kits since the pandemic hit.
CP: What is one thing that you see missing from discussions about COVID-19?
LP: The truth of the historical medical racial trauma of black folx by the medical community and healthcare systems. People discussed the lack of "compliance" and the need to recruit for vaccine studies due to underrepresentation but no one discusses the density of the trauma that lead to the well earned distrust of black people in STL. Restorative justice requires us to first acknowledge the bad things we have done to people if we hope to create equity. I wish I heard more acknowledgement of that history and less of a disbelief about why folx don't trust. You can't beat someone down for centuries and then wonder why they don't jump when you say jump, even if the building is truly on fire.
CP: What is something giving you hope right now in terms of COVID-19?
LP: The way that systems are collaborating and bending to create new community based solutions. PrepareSTL is a model of a multi agency community based solution to distribution of health education and resources that is just amazing. The pandemic task force is another great example. And places like BJC bringing on new leadership levels with people like Dr. Player and Purnell is just refreshing.