This week’s edition of River City Data is the last for November.
If you missed it, a special edition of River City Data went out yesterday with an in-depth, “FAQ” style discussion of schools and COVID-19. This will stand-in for my usual “In the Weeds” section. I’m very grateful for my SLU PRiME colleagues Kristi Donaldson and Evan Rhinesmith as well as my SLU AHEAD colleague Tim Wiemken for collaborating on this special issue.
In tonight’s newsletter, I give an update on the dire situation in Missouri, break down the latest numbers, and share my interview with Springfield-based CoxHealth President and CEO Steven D. Edwards.
- Chris
COVID-19 by the Numbers
Total cases in MO: 270,486 (+29,250 from last Friday)
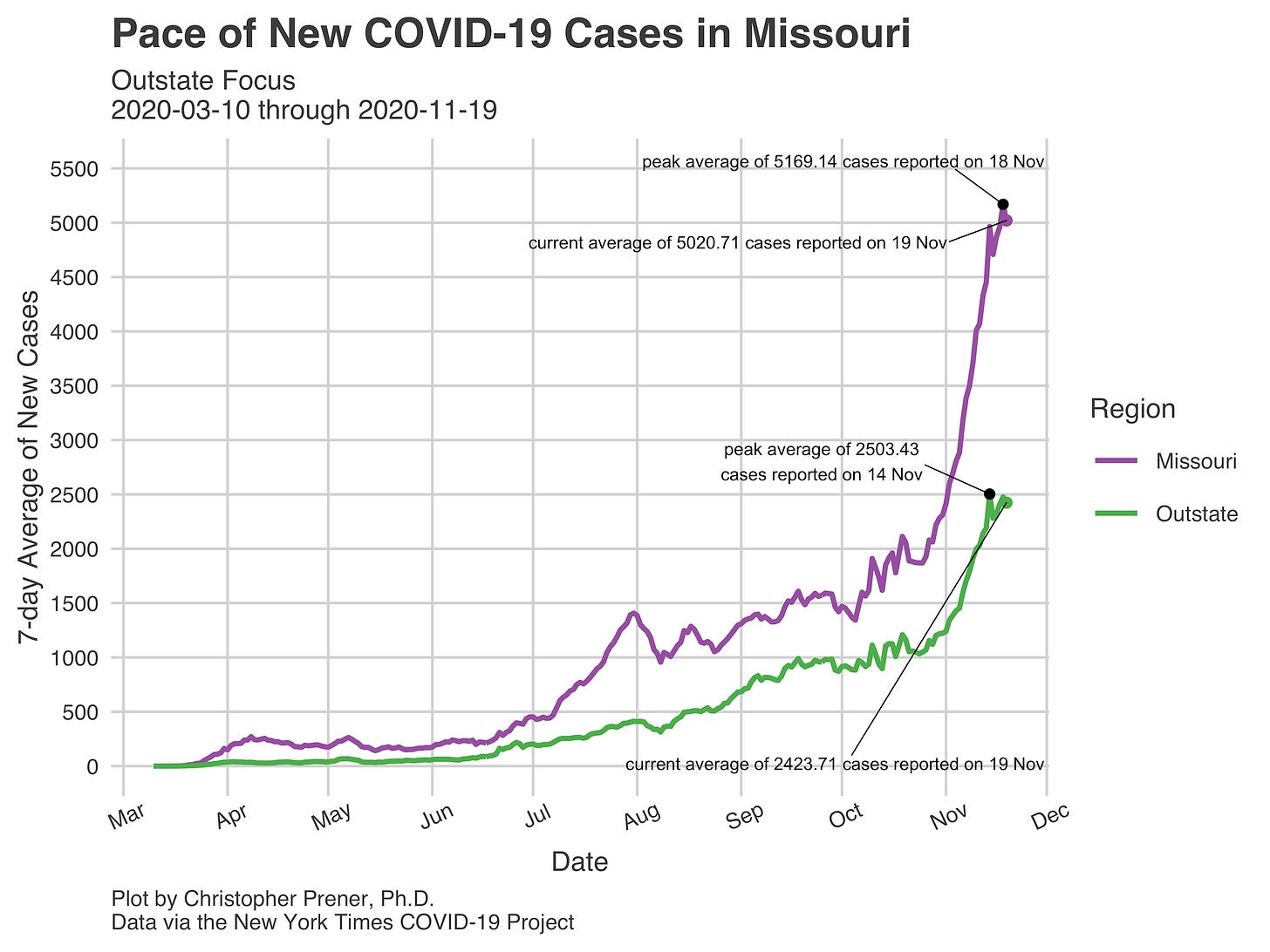
7-day average of new cases per day in MO: 5,020.71 (+566.14 from last Friday)
Counties with the highest per capita rates of new cases per day this past week:
Perry (171.61 per 100,000), Pettis (160.15), Nodaway (154.6), Cape Girardeau (150.66), Henry (148.99), and Gentry (147.89)
Total deaths in MO: 3,618 (+166 from last Friday)
7-day average of new deaths per day in MO: 25.29 (-8.29 from last Friday)
These numbers are current as of Thursday, November 19th. Additional statistics, maps, and plots are available on my COVID-19 tracking site.
Summary for the Week Ending November 20th
This past week saw considerable growth in new cases here in Missouri. The 7-day average yesterday was over 5,000 for the first time ever. I’ll note for folks (again) that comparisons with trends before August are not apples to apples because of differences in the numbers of tests administered weekly. Since August, however, the number of tests administered has been relatively stable. This makes the precipitous rise in cases statewide, and in the “meso” regions I track cases in, all the more notable.
Per capita, the rates of new cases are highest in the broad (and rather fictitious) “outstate” region. Based on the map of county-level rates of new cases below, areas of particular concern are Southeast Missouri and the Bootheel, Mid-Missouri, and in a wide range of counties throughout Northern Missouri.
You’ll notice from the map that rates of new cases in the metro St. Louis area are highest in St. Charles County right now. Lincoln, Jefferson, and St. Louis counties are all slightly below that rate but still quite high. While new case rates in the City of St. Louis are indeed up, they remain well below surrounding counties. I would not take solace in this relatively low rate, however. As you can see below, even the City with its low rate is trending upward. So while rates of new cases are relatively low, they’ve jumped to a level five times higher than they were in early October.
One consequence of this can be seen in the hospitalization rates within the St. Louis Metro. For the first time in the pandemic, there are more than 1,000 confirmed and suspected COVID-19 patients in St. Louis hospitals this evening, with no sign of growth in that trend abating.
These hospitalization numbers, combined with the volume of new cases being identified, is why I described the situation in Missouri as dire in the intro to tonight’s newsletter. St. Louis is not the only region struggling in Missouri, either. In the Springfield area, there are now more than 200 individuals who have been hospitalized. There are concerns that these numbers, like in St. Louis, will continue to grow.
Back in St. Louis, the Pandemic Task Force is discussing using National Guard soldiers in non-clinical roles and preparing crisis standards of care. These protocols would be used to determine which individuals would be prioritized for potentially life-saving treatment. They provide a roadmap for health care providers to follow if demand for ICU beds, ventilators, or other interventions outpaces capacity.
The biggest challenge right now is not necessarily beds themselves but people to staff them. While the National Guard does have clinical personnel, they’re already committed to their local communities. Activating them would only rob those communities of already scarce health care providers. So, while the State may be considering setting-up field hospitals, my friend Gregg Favre points out that we cannot rely on the Guard to staff them.
The best thing we can do right now to support these health care providers is not to figure out how to staff field hospitals (though we may not have a choice) but rather reduce transmission. Wearing masks, avoiding all non-essential indoor activities with people from outside your household, not dining in restaurants (get takeout!), and working from home are crucial strategies. On Thanksgiving, the safest thing you can do is not eat indoors with anyone outside your household.
Weekly Interview
This week’s interview is with Steven D. Edwards, the President and CEO of CoxHealth, a private not-for-profit healthcare system operating 6 hospitals and over 85 clinics in Southwest Missouri in and around Springfield. He is a 1988 graduate of Drury University, completed an MHA from Washington University in 1990, and a post graduate fellowship at Baylor University Medical Center in 1991. Prior to returning to CoxHealth in 1992, Mr. Edwards worked at Baylor University Medical Center, and Barnes-Jewish Hospital.
CP: What has it been like being a hospital CEO during the COVID-19 pandemic?
SE: This is the city [Springfield] where I grew up, filled with the people I love, which makes this work immensely more personal and significantly more weight bearing to me. In March we took the perspective that if we were given a warning that a natural disaster was coming, and we might have anywhere from a few weeks to a few months to prepare, and our preparation could save or cost the lives of people we loved, how hard would we work? That was the attitude of our organization, and I am proud of the response of our team. Their preparation was relentless. This has been a battle, there is no separation between work and home, I imagine it is what a wartime officer might feel. I hope that when we overcome this disease, people will know that I, along with others, fought our hardest for our hometown and region.
CP: What are the biggest challenges you are facing right now as a hospital system?
SE: In March we broke our response down into four categories 1) Suppression. 2) Space. 3) Stuff. 4) Staff. We have fought hard to drive political leaders to take the appropriate non-pharmaceutical interventions, and while we had success in Springfield, Branson and a few other cities, we are still an island or masking surrounded by a sea of non-maskers. This is a major failure. We have been successful dealing with space issues, adding up to 146 beds by the end of this month to our main hospital campus. We built up our supplies of PPEs, medicines other important tools. Our biggest challenge right now in the incredible demands this pandemic places on hospital staff.
CP: How has your COVID-19 response affected your staff, and are you worried about burn-out and long-term staffing issues?
SE: Last week, in one night, we lost eight patients. While healthcare is filled with resilient people, the long term impact of fighting this disease will be heartbreaking and there will be emotional scars. Yet, I do think that the sense of mission is more powerful today than ever, and it will continue to draw heroic and like-minded people into our field.
CP: What is one thing that you see missing from public discussions about COVID-19
SE: Too often civility has been missing in a polarizing election year. [Editor’s Note: public health officials across Missouri and the United States have resigned after being threatened and harassed over COVID-19 policies and restrictions.]
CP: What is something giving you hope right now in terms of COVID-19?
SE: I am filled with hope and I think it is well founded. We are seeing an incredible global commitment to vaccine development which has accelerated beyond what I thought was fathomable. We have seen science take a novel disease and learn and disseminate knowledge at unprecedented pace. For a brief period in the shutdowns we were amazed how quickly nature can repair our damage, which gives me hope that we can learn to repair our planet. I have seen the “helpers” that Mr. Rogers referred to in a crisis rise up heroically. At times this pandemic has challenged my faith in humanity, but my faith remains intact.