I’ve been thinking a lot lately about how well prepared we are for what comes next. There is a sense (including the President and Vice President) that we could not have foreseen the Delta and Omicron waves. Just a few weeks ago, Missouri Governor declared that the state of emergency was no longer needed even as health care systems, which relied on provisions in the state of emergency, warned him otherwise.
In my tweet about this lack of imagination today, I referenced a scene in the 2001 film “Spy Game” where Robert Redford’s character discusses the need to plan far ahead and imagine the worst-case scenario. Noah built the ark before the rain began, he reminds his assistant. Unfortunately, what is happening right now in St. Louis, Missouri, and the United States is an utter failure to anticipate a wave like Omicron despite the clear warnings from public health leaders that it could happen.
We need to take stock of where we are right now (which I do below) not just because it is of immediate relevance, but because this is an opportunity to learn the lessons we have failed to realize after past waves. Though New York’s Governor Hochul sees a “glimmer of hope” in her state’s data, we cannot promise this will be the last wave. So, we should prepare as if it will not be. Moreover, we need to prepare as if the next wave will be even worse. To return to Robert Redford, as we work through the challenges of the current wave, we simultaneously need to prepare for torrential rain that far exceeds the Omicron surge. - Chris
COVID-19 by the Numbers
Total cases in MO: 1,150,130 (+79,740 from last Thursday)
7-day average of new cases per day in MO: 11,391.43 (+3,345.43 from last Thursday)
Counties with the highest per capita rates (per 100,000) of new cases per day this past week:
St. Charles (284.37 per 100,000), Kansas City (258.23), St. Louis (254.89), Lincoln (254.54), Warren (233.4), Boone (224.99), St. Louis City (223.97), Jefferson (212.97), and Jackson (211.64)
Total deaths in MO: 16,754 (+305 from last Thursday)
7-day average of new deaths per day in MO: 43.57 (+8.71 from last Thursday)
Percent of all Missourians initiating vaccination: at least 57% (+1% point from last week)
Percent of all Missourians completing vaccination: at least 51% (+1% point from last week)
Case and mortality numbers are current as of Wednesday, January 12th. Vaccination numbers are current as of Thursday, January 13th. Additional statistics, maps, and plots are available on my COVID-19 tracking site.
Trends in the Past Week
The list of counties with high rates is just astounding right now. Nine counties with rates above 200 new cases per 100,000 people per day on average over the last week. That’s about 2,500 new cases per day on average in St. Louis County alone. Boone County is the only county in that list not in either the St. Louis or Kansas City metros. You can see clearly how unprecedented this volume of new cases is when you step back and look at the rates regionally. The overall rates in both the St. Louis and Kansas City metros are over 200 new cases per day per 100,000 residents, while “Outstate” Missouri’s rates about half this rate though still at an all-time high. These dwarf our prior all-time highs, from November 2020, in dramatic fashion.
The rates in “Outstate” Missouri are tricky. Yes, they are quite a bit lower. But look how many counties we have with 106 new cases per day per 100,000 residents on average - every region of Missouri has counties in the third bin or higher on the map. So, we can find levels of high transmission can throughout the state.
The rates are at or above all-time highs from prior surges in many cases. For example, this is true in Boone County as well as Callaway, Cole, Gasconade, and Montgomery counties in Mid-Missouri. It is important to note for Boone, in particular, that the University of Missouri has not yet returned to in-person classes. Without a campus mask or vaccination mandate in place, their classes begin on Tuesday.
One of the complicating factors with Omicron has been the oft-repeated news that this variant of the virus is milder. Unfortunately, this has led folks to assume that the case counts are not the metric to focus on or that we might see a divergence between case counts, hospitalizations, and mortality.
At the end of December, which is the most recent statewide hospitalization data we have, we were in the midst of converting to a majority of new cases being from Omicron instead of Delta. So, the hospitalizations this plot captures are, by and large, likely to be Delta infections. But, critically, this is the second wave of Delta hospitalizations - the spikes visible in all of our metros during the summer and early fall of 2021 were the first.
So, on New Year’s Eve, hospital staff were exhausted. Not just twenty-one months of a pandemic, but six months of Delta-fueled hospitalization surge. What has happened since, however, is that our hospitalizations in St. Louis and elsewhere have continued to climb. In St. Louis, we are currently adding new patients at an unprecedented clip.
Overall hospitalization numbers in St. Louis have far outstripped our prior all-time high, with several one-day numbers (including suspected COVID patients) coming it at over 1,400 patients. So, not only were hospital staff already exhausted by New Year’s, but we have now moved well beyond those already high hospitalization numbers.
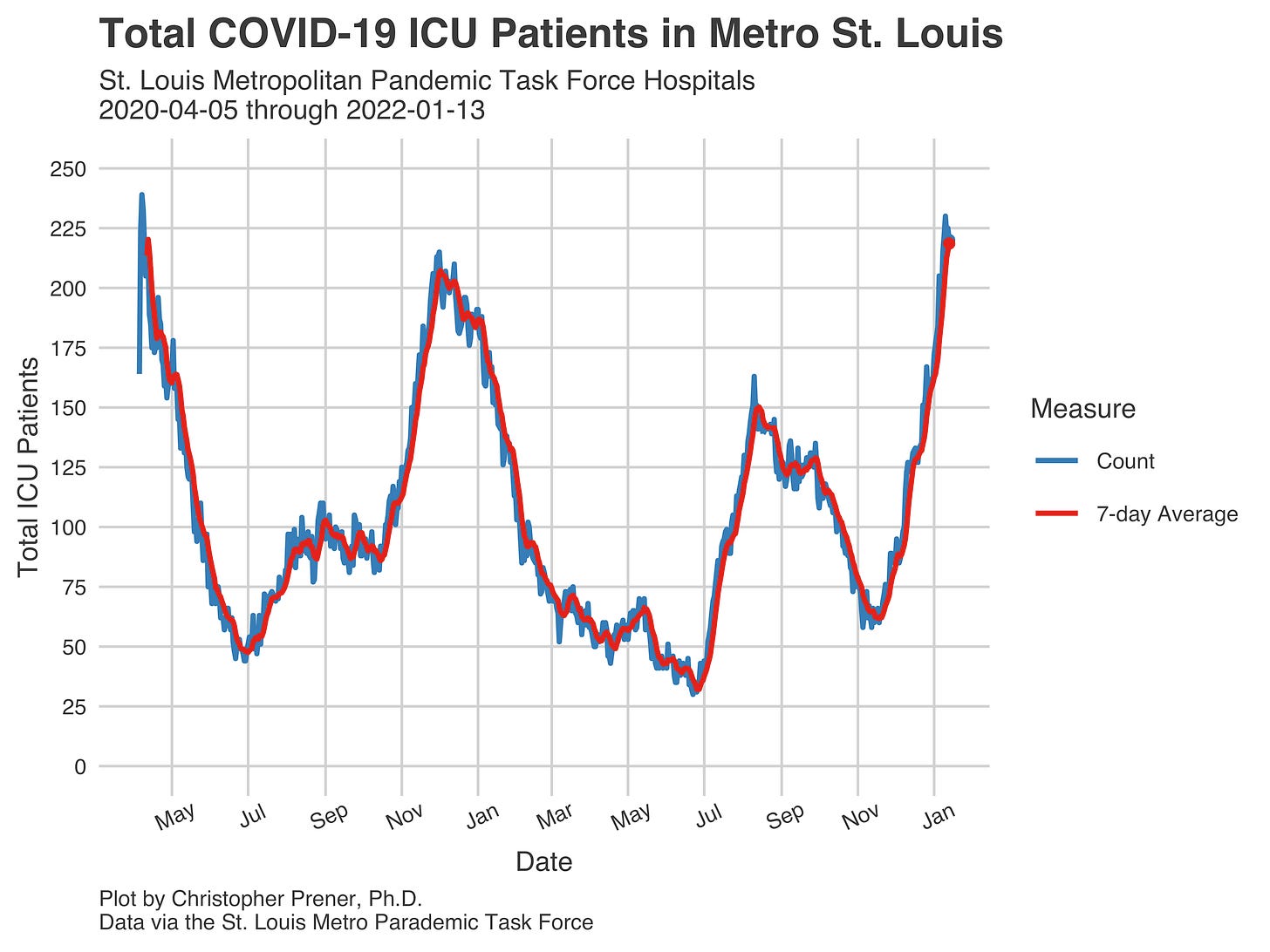
Worse still, our ICU numbers rival those that we saw in the very first wave of the pandemic. We are less than two patients, on average, below that all-time high, and we may surpass it this week.
So, what is going on here? One possibility is that there is still a significant share of patients infected with the Delta variant in ICUs. The other is that, while Omicron is milder, on the whole, it can still create severe symptoms for patients. Given how many people are testing positive right now, even a small number of patients requiring hospitalization can create significant pressure. So, while the ratio of ICU patients to all COVID patients has never been lower, the sheer number of patients means that our ICU numbers are still quite high.
This point gets me back to my introduction, referencing the Robert Redford film. Imagine for a moment that we faced a variant that was as transmissible as Omicron but caused severe illness like Delta did. Check out the ratios in the plot above - other than our initial wave, we had the highest share of hospitalized patients requiring ICU care and mechanical ventilation during our first Delta wave. What if that was now? This hypothetical is just that, but we need to prepare for it as a country and a state.
There are no guarentees with COVID-19’s evolution, and policymakers wasted precious time this spring planning for “reopening” our economy and getting past the pandemic. Instead, we are enduring the most severe challenges we have faced yet from COVID-19. Only now is the White House ordering a billion at-home tests. High-quality masks have not been made freely available. Schools and services are struggling to stay open. We need to ensure this is the last wave where we are caught flatfooted. Worse still, if there is a next time, more health care providers will have joined the great resignation or have internalized the trauma of this wave. We need to be clear-eyed about future risks, even as we respond to the current crisis.