Tonight edition includes an update on COVID-19 trends in Missouri, my first look at racial disparities in vaccine doses in Missouri’s Region C (which includes St. Louis), and my interview with SLU Medical School Assistant Professor Dr. Sarah Gebauer, who has been working on and off on COVID-19 rotations at St. Mary’s Hospital in St. Louis. As always, I hope you find these data and Dr. Gebauer’s interview useful! - Chris
COVID-19 by the Numbers
Total cases in MO: 511,506 (+3,901 from last Friday)"
7-day average of new cases per day in MO: 694.14 (-241.71 from last Friday)
Counties with the highest per capita rates of new cases per day this past week:
Scotland (29.17 per 100,000), Christian (24.58), Butler (22.06), McDonald (20.65), Clark (18.91), Callaway (18.16), Lincoln (17.74), Clay (16.78), and Jackson (16.2)
Total deaths in MO: 8,087 (+247 from last Friday)
7-day average of new deaths per day in MO: 41.29 (-1.57 from last Friday)
These numbers are current as of Thursday, February 18th. Additional statistics, maps, and plots are available on my COVID-19 tracking site.
Summary for the Week Ending February 19th
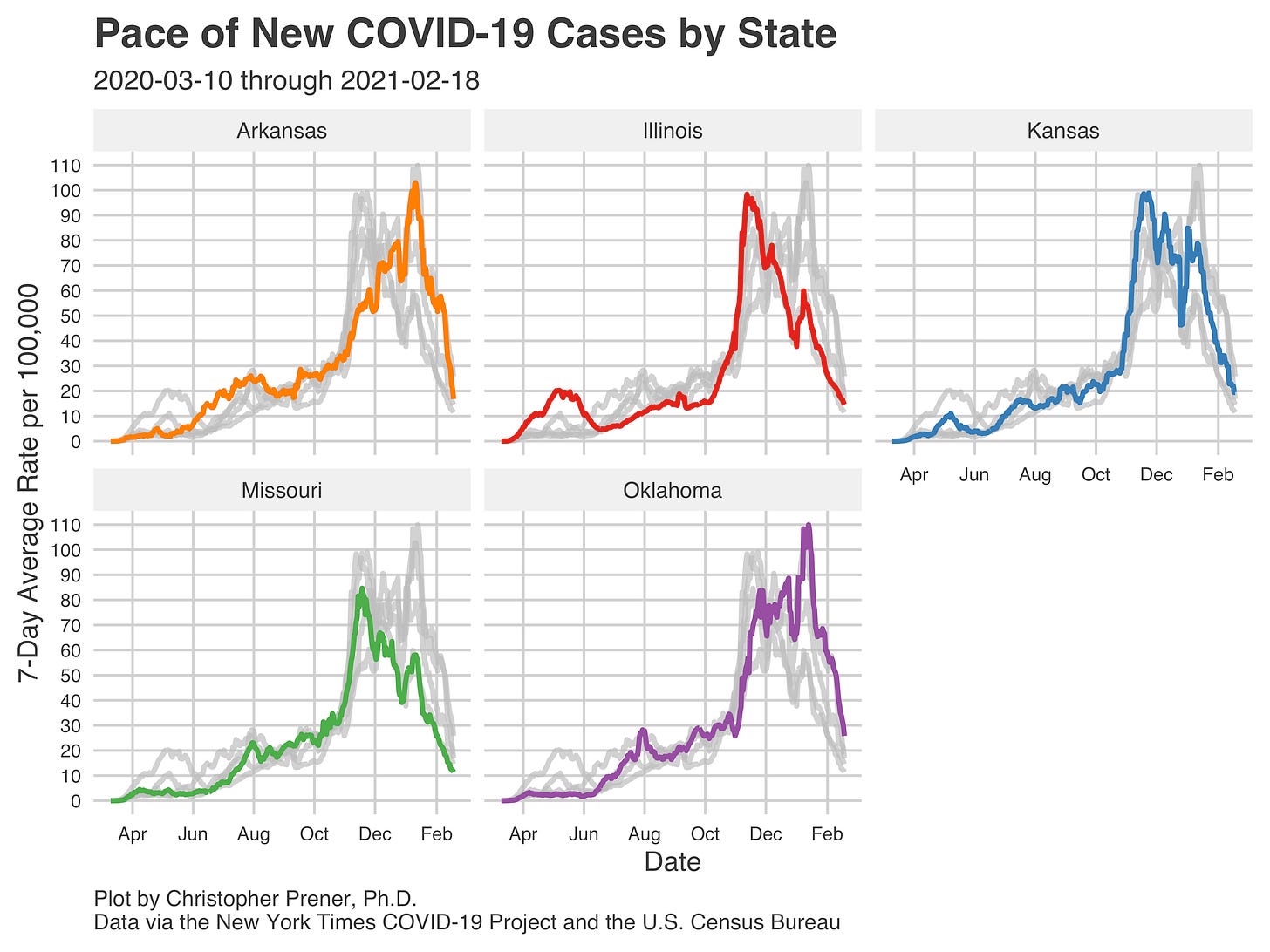
Missouri continues to see declines (though at a slower rate) in the numbers of new cases across the state. ur rate of new cases now is roughly where it was in July 2020. For those who remain skeptical of these trends, I’ll remind folks that these declines largely mirror the trends we see in neighboring states.
Another piece of evidence that supports the narrative of declines is the shift in hospitalizations in St. Louis. The numbers of total in-patients have dropped substantially, with our 7-day average number of in-patients sit on the low side of our plateau between July and October of last year.
One data point that I do not have on a plot is the total number of discharged patients from St. Louis hospitals. The number is eye-catching - likely tomorrow, we’ll have discharged more than nineteen thousand patients since the beginning of the pandemic.
These declines mean that even the counties being hardest hit with new cases right now are only being hard hit in relative terms (see the list in the prior section and the map below). The top-level rates in Scotland, Christian, Butler, and McDonald counties are well below their peak values from a few months ago.
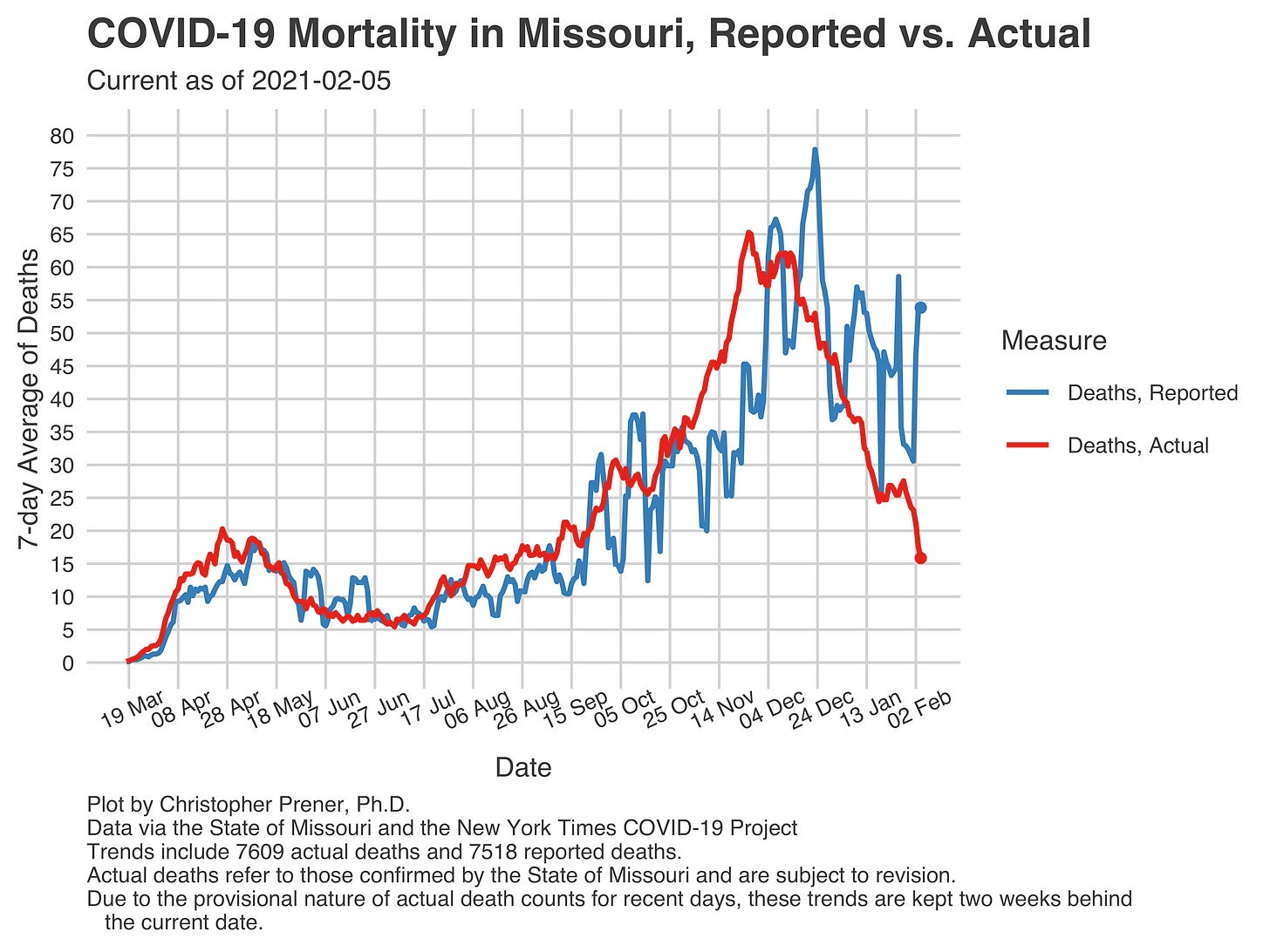
Another eye-catching number from this week is Missouri's total mortality rate. We passed eight thousand deaths a few days ago, with late November and early December being the pandemic's deadliest period so far. We were averaging between fifty-five and sixty-five deaths per day during those weeks.
These death data are incomplete, and the rate shown here for late January is likely artificially low and fails to capture the consequences of the post-holiday bump in new cases. Nevertheless, it shows the same rate of improvement that we have seen in the numbers of new cases and hospitalizations.
Vaccination Update
The St. Louis Pandemic Task Force has again released an update on vaccination delivery and results to date. The breakdown of doses for the coming week is the same as last week’s. To date, 311,722 vaccination doses have been administered.
I also have my first COVID vaccination plot to share. This is based on data of the race of vaccinated individuals that the Task Force has been releasing weekly. Instead of presenting these as percentages, I have converted them into estimated per capita rates. These give a far better sense of the magnitude of racial disparity in vaccination rates here in St. Louis. The picture is devastating, with doses being given to white residents of Region C at more than twice the Black residents' rate.
Region C includes Pike, Lincoln, Warren, St. Charles, Franklin, St. Louis, Jefferson, Washington, St. Francois, Ste. Geneviève, and Perry counties as well as the City of St. Louis.
Into the Weeds
While the pandemic is still unfolding around us, we got a stark picture of the effect it has had on life expectancy in the United States this week. Over the first half of 2020, African American men's life expectancy declined by three years, while Latino men’s life expectancy dropped by just under two and a half years. These reflect the ways that both gender and racism influence outcomes with COVID.
Weekly Interview
Dr. Sarah Gebauer is a physician who is board-certified in family medicine. She is also an Assistant Professor at Saint Louis University School of Medicine. Over the past few months, Dr. Gebauer has been working on COVID-19 details at St. Mary’s Hospital in Richmond Heights.
CP: You spent part of December on the St. Mary’s Hospital COVID team - can you tell us a bit about what the experience was like personally - what was it like for you to serve on that team?
SG: I got notice that we were "putting the band back together" in November, as the COVID-19 numbers were increasing and our colleagues were requesting that Family Medicine run a supporting COVID team. I had helped in April and had anticipated that I would be asked to help again. I volunteered to work on the service, as I'm one of the lowest risk members of the faculty and felt this was an important place I could help and potentially protect my more vulnerable colleagues. The most heartbreaking moment for me was talking to my 9-year-old son about it. We were watching the local news, which was showing inside COVID wards and I turned and told him, "See that place, Buddy? I'm headed back in there next week." He got scared and it tore me apart. I reassured him that I had gotten through one week before safely and I'd do my best to do so again. Another challenging aspect is isolating myself from my family while I work on the wards. I try to limit physical contact, which is difficult for my family to endure, especially my children.
CP: Can you share generally what types of medical issues you saw with folks who were hospitalized at St. Mary’s? I’m interested in sharing what the things are that lead to hospitalization for COVID patients.
SG: The most common things we saw were COVID pneumonia. COVID is different from viruses like Influenza in that it causes a unique viral pneumonia that is very characteristic on chest x-ray. These patients usually are extremely short of breath and require oxygen. I've also had patients with GI symptoms (nausea, vomiting, diarrhea) as well. A typical hospitalized COVID patient is hypoxic (has low blood oxygen) needing oxygen supplementation and is very debilitated. So many end up needing to go to a nursing home or a rehab facility to get stronger before it will be safe to go home. We talk a lot about COVID death rates, but we don't spend as much time on the consequences such as prolonged or permanent debility. It's very difficult for patients and families to grapple with the loss of independence.
CP: More generally, what has the pandemic been like for you in your role as a primary care provider?
SG: Providing primary care has certainly been challenging. Early in the pandemic, we essentially crashed onto telehealth. Finding ways to ensure my patients got the chronic care they needed, but also mitigating the risk of in-person appointments was and is difficult to balance. As the weather changed and we saw an uptick in respiratory symptoms, we had the additional challenges of how to safely evaluate patients that could have COVID-19. I work with uninsured populations, which adds an additional layer of challenge, as they may not have access to affordable care anywhere else. Like most primary care settings, we're still working out the best practices. Necessity is the mother of invention.
It's also difficult to maintain relationships with patients when you can't see them in-person. Relationships are the bedrock of a therapeutic relationship, with trust at the center. Ensuring my patients know how much I care for them and that we are working hard to keep them safe is a priority.
CP: There has been a lot of discussion about the vaccine, and given that you work as a primary care provider, how are you communicating about the vaccine with your patients?
SG: I approach it from a few different directions. When patients ask about it, I'm always quick to disclose that I have been vaccinated and share my experiences getting the vaccine with them. I explain how I came to trust the vaccine, which was a thorough review of the data presented publicly during the Emergency Use Authorization. My vaccinations were uneventful, a sore arm after the first one, and a sore arm, fatigue, and headache after the second. I found this reassuring, as it indicated an immune response (at least to me).
However, it's also important to acknowledge hesitancy and that feeling that way is understandable. This is particularly important with communities of color. As a white woman, sometimes my voice isn't the right voice. In those situations, I have been referring my patients to clinicians and public health professionals of color, who relate their experiences with the vaccine and how they came to trust in the technology.
CP: Finally, what is giving you hope right now in terms of where we are at with COVID?
SG: I think I have two big sources of hope for a "Post-COVID World" right now, or at least a manageable COVID world. One is in the vaccines. Early data are extremely strong that these vaccines are outstandingly effective and that there are several more in the pipeline. Second, are other nations that have managed to control the outbreak well. This inspires me in demonstrating that it can be done if we all work together and move in the same direction.
If you like what you see here and don’t already, please subscribe!