In tonight’s edition of River City Data, I break down the latest trends and numbers, provide my most detailed update on vaccination trends yet, and share my interview with Dr. Rachel Winograd about how the pandemic has affected another major public health issue, the use of opioids. - Chris
COVID-19 by the Numbers
Total cases in MO: 515,808 (+3,536 from last Friday)
7-day average of new cases per day in MO: 614.57 (-52.14 from last Friday)
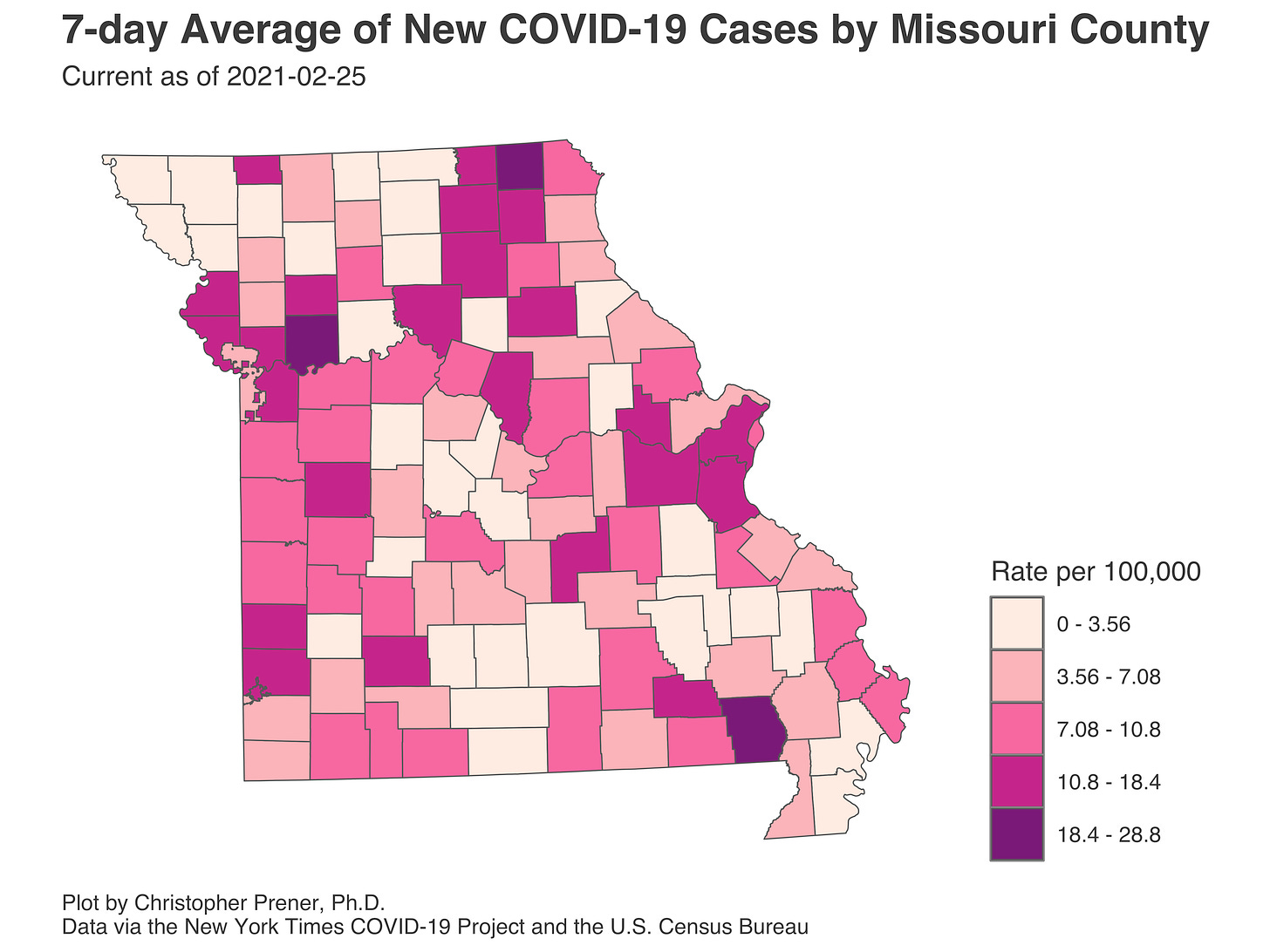
Counties with the highest per capita rates (per 1,000) of new cases per day this past week:
Ray (28.79 per 100,000), Butler (22.4), Scotland (20.42), Greene (16.34), St. Louis (14.96), Knox (14.46), Clay (14.33), Phelps (14.03), and Worth (14.01)
Total deaths in MO: 8,355 (+215 from last Friday)
7-day average of new deaths per day in MO: 38.29 (-4.57 from last Friday)
These numbers are current as of Thursday, February 25th. Additional statistics, maps, and plots are available on my COVID-19 tracking site.
Summary for the Week Ending February 26th
There is very little to report in terms of new cases in Missouri right now. As you can see just above, only three counties have a per capita rate of over 20 new cases per 1,000 residents right now. That’s a startling decline from our highs in November and even from where we were in early to mid-January.
I find it really striking to consider that the St. Louis metro counties in Missouri were adding an average of over 1,800 new cases per day in mid-November. Fast forward two months and the entire state is averaging just a third of what seven counties were seeing before Thanksgiving.
I would be remiss if I did not remind folks, however, that since Thanksgiving, our increased reliance on antigen testing without reporting those results at the county-level means that December, January, and February numbers are all biased downward by somewhere between 25% and 30% of what they should be (that is back of the napkin math, for what it is worth). Even at 30%, however, that would mean we are averaging right around 800 new cases per day right now. This is a pretty impressive improvement, though I cannot point to a single factor driving this.
The three highest rate counties, the only three with per capita rates over 20, are on different trajectories right now. Butler County, in Southeast MO, has had much higher rates but has not seen them drop towards zero as other Bootheel (and Bootheel adjacent) counties have. Scotland County, in Northeast MO, did have its cases drop to near zero after the post-holiday bump but has seen a small resurgence in new cases. Finally, Ray County, near Kansas City, is seeing a spike driven by double-digit numbers of new cases on one day in the past week.
These really are the outlier counties, though. The typical county has been cases subside. We see these trends mirrored in our neighboring states, though Arkansas is experiencing a notable recent uptick in new cases.
I point this out to underscore that this is not just about Missouri omitting antigen tests but rather a durable pattern that mirrors other durable patterns in neighboring states.
Vaccination Update
There are three new vaccination plots that I want to share tonight. The first, which I’ve been putting out on Twitter this week, shows the geographic dispersion of vaccine administration by county in Missouri. The lowest rates of first dose immunizations are in Southwest Missouri and the Ozark Mountains, with relatively low rates in both the Kansas City and St. Louis metros. Counties like Cape Girardeau and parts of Mid, Northwest, and Northeast Missouri have the highest per capita rates.
These come despite the State’s assurances that regions of Missouri are receiving equal numbers of doses in weekly shipments. The problem with this narrative is that there is a disconnect somewhere, either in the State’s narrative or in the process itself. We can see this in first dose rates by Missouri State Highway Patrol District, which is how vaccines are being distributed. This is a brand new plot I put together tonight:
District I, just to the southwest of St. Louis, has administered more than sixty fewer first doses per 1,000 individuals than District F, which covers Mid-Missouri. Districts C and A, which cover St. Louis and Kansas City, have both administered about forty-five fewer first doses per 1,000 individuals than District F.
I am not sure where the breakdown is. It could be that deliveries of doses to Districts are not going out as equitably as the plan for each week makes it seem. It could be that vaccination providers are more efficient in some Districts than others. Perhaps clinics are better advertised in some Districts, or it has been easier to access them. I am really not sure. What I do know is the idea that Districts are administering vaccines at equal rates is not borne out in the data.
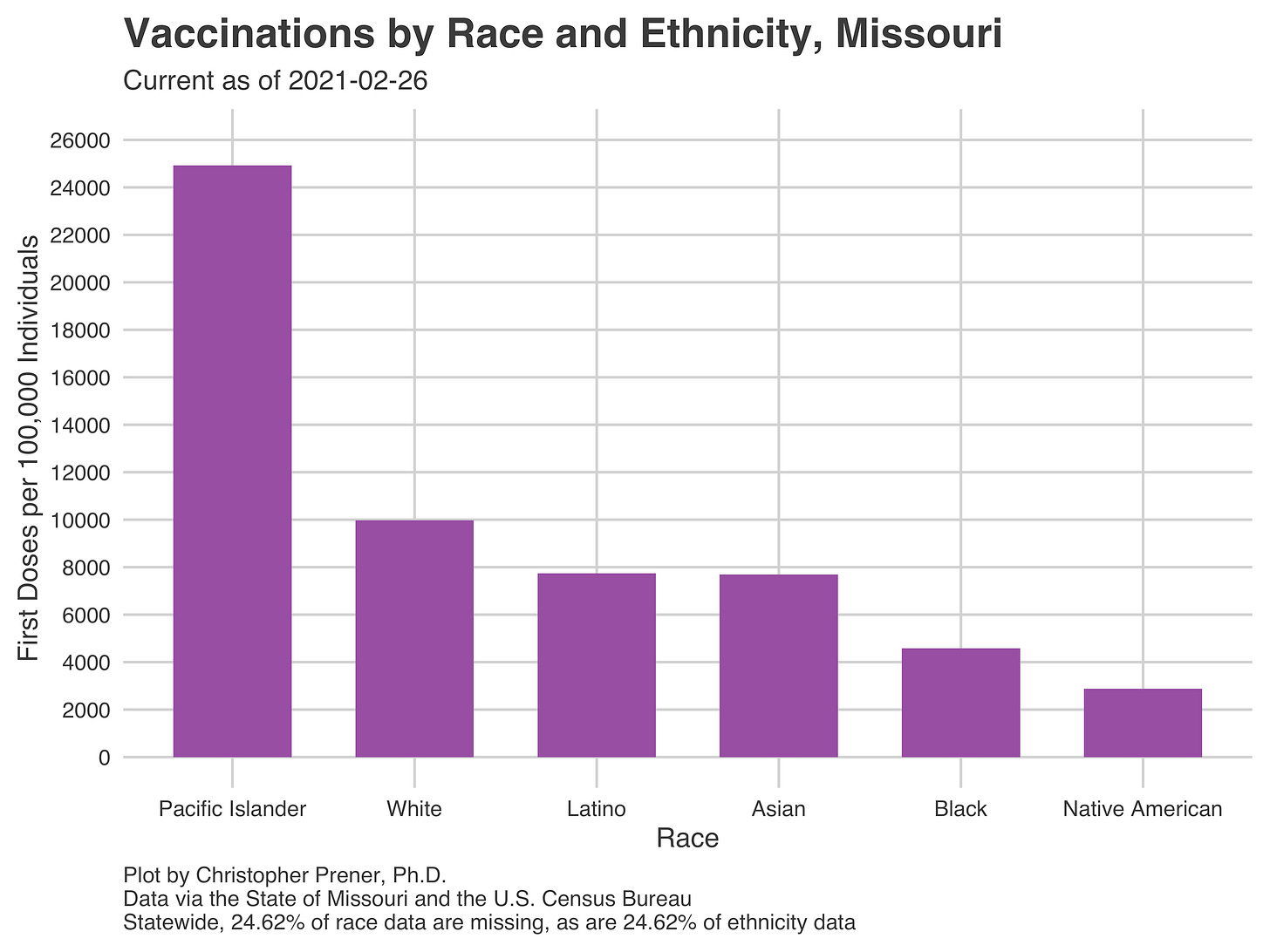
Disparities with vaccinations also extend to race and ethnicity. White Missourians are receiving first doses at roughly twice the rate of African Americans and four times the right of indigenous Missourians. I have been sharing this plot this week on Twitter as well:
Taken together, these data paint a picture of the challenges ahead for Missouri in getting communities vaccinated, both in terms of who is being given first doses and where they live.
Into the Weeds
One question to ponder with decreasing counts of new cases and increasing vaccinations is "when we get back to normal?” The answer is complicated, as this article in The Atlantic describes. There are many questions about what the spring looks like, with the potential for an increase in cases as states try to reopen and new variants become more widespread. According to the article, there is some agreement that conditions this summer may allow everyone to relax a bit. However, it may be only a temporary reprieve with the potential for a fall and winter 2021-2022 spike in new cases yet again.
Weekly Interview
Dr. Rachel Winograd is an Associate Research Professor at University of Missouri St. Louis – Missouri Institute of Mental Health. Her clinical, research, and program development interests revolve around interventions to save and improve the lives of people who use drugs. Currently, her primary focus is on expanding access to medical treatment, harm reduction strategies, and culturally-responsive services for those most in need of evidence-based care for substance use disorders in Missouri. Contact her at rachel.winograd@mimh.edu or follow her and the noMoDeaths team on Twitter.
CP: Tell us a little bit about where things stood with opioid use before the pandemic - what patterns were you seeing?
RW: Prior to the onset of COVID-19, we were beginning to see the overdose crisis move in a positive direction in Missouri and St. Louis, at least overall. Drug-involved deaths were down 3.4% in the state in 2019 and down 7% in St. Louis (city and county) – the first decreases we’d seen in years.
Critically though, this decrease was not experienced equally across groups; deaths among Black men continued to increase in 2019. In the St. Louis area for example, opioid-involved deaths among White men decreased 23% between 2018 and 2019, but increased 17% among Black men (including a startling 46% increase among Black men in St. Louis County). This increase in deaths among Black men in particular has been ongoing since 2016, though deaths were also increasing (though at lesser rates) in other demographic groups, so it was less stark of a disparity than what we saw in 2019.
Regarding opioid use in general, we have not necessarily seen an increase in the *number* of people who use opioids in the last 5 or 6 years. Instead, the overdose crisis has been driven by a more potent and deadly drug supply (so even if the same number of people are using drugs, each use comes with a higher risk of death). Specifically, illicitly-made fentanyl really took over the St. Louis drug supply in 2016, and that’s when we saw deaths jump up most dramatically. We have also seen deaths involving methamphetamine go up – usually in combination with fentanyl, but not always. For these reasons and others, many of us in the field prefer not to call what we’re experiencing an ‘opioid crisis’ as much as it is a ‘poisoning crisis.’
CP: Since COVID-19 and the lockdown, how have things changed? Why do you think these changes have occurred?
RW: Regarding drug-related fatalities, overdoses increased dramatically in April and May in the St. Louis region (as well as throughout Missouri and the U.S.). Reasons behind this range from very internal (increased stress, isolation, loneliness, depression) to circumstantial and external (support services were less available, drug supply was more potent and less predictable, people lacked access to basic needs like housing and food). At this point it does seem like overdose rates ‘stabilized’ (which is not really the right way to say it, since every overdose death is a preventable tragedy) in the latter half of 2020, perhaps because access to services went back up, the drug supply leveled out, or – and this is the darkest possibility – those who were most vulnerable and at-risk of death had already passed away in the early months of the pandemic.
In terms of addiction treatment services specifically, we saw a rush of loosened federal regulations in March and April of 2020, designed to make virtual treatment more accessible and reduce the need for in-person services in crowded clinics. This included allowances to start buprenorphine with a telephone visit, taking home two or four weeks of methadone doses at a time, waived requirements for physical client signatures, etc. It’s too early to know the impact of these changes on, for example, the volume of virtual/audio visits (we can presume they went up) and the corresponding clinical impact of transitioning in-person services to virtual, or initiating and continuing care in an exclusively virtual format. Most treatment and recovery programs did seem to revert back to in-person services relatively soon after the lockdown, for multiple reasons (clients didn’t have the smartphones/data plans/chargers they needed, some people preferred in-person services for human connection, clinical programs weren’t set up to be all virtual, etc.).
CP: I’m interested in your perspective on how street outreach, harm reduction, and other typically face-to-face interactions have been affected by the pandemic.
RW: I must say I was incredibly impressed and inspired by the way so many harm reduction and other service providers pivoted to meet the needs of the people they served. Street outreach activities, naloxone and sterile syringe distribution actually increased – folks were out in mobile units, on foot, posted up at testing sites and food giveaway events – getting very creative to make sure they were reaching as many people as possible. These individuals were also being incredibly flexible and trying to address the multiple and intersecting needs of community members in a single exchange. Take for instance the team at The T under Dr. LJ Punch, they’ve been giving out not only naloxone, but also masks, bottled water, hot hand warmers, even hot dogs. For most people who use drugs, that drug use is just one part of their lives. They may need help with it, but they need help for other things too.
While street outreach increased, open drop-in hours at brick and mortar locations decreased or stopped completely. Of course this has been a major loss, especially since people often utilize harm reduction and recovery services not just for the naloxone, syringes, or other supplies, but for the community, comradery, and connection they provide. It’s hard to replace the comfort people can get from a couch and a cup of coffee and sitting around with others who are going through the same things they’re going through. In this sense it’s a reminder that people who use drugs are missing the same things everyone else is missing; the days when we could be physically together and share each other’s grief and joy without worry that we or someone we love would get sick.
CP: From a policy standpoint, has COVID-19 changed how you think we should be addressing the opioid use epidemic in Missouri?
RW: The impacts of the pandemic and all its ripple effects, economic and otherwise, have really brought into focus the need to address the overdose crisis in ways we had begun to do pre-pandemic, but not with as much urgency as was needed. Specifically, the need to make addiction treatment more flexible, accessible, and available has become abundantly clear. This comes in concert with the need to change reimbursement structures, regulations, and oversight in such a way that low-barrier treatment options are plentiful and practical from the standpoint of those charged with providing such services. We also must be doubling down on addressing the growing racial inequities we are seeing not only in overdose deaths themselves, but in engagement in substance use services, the location of these services (there are barely any in North St. Louis County, for example), and the racial makeup not only of people providing these services but those who are making the big decisions about what, where, and how these services are provided. Last, we need to have an even greater appreciation for how intertwined our safety net systems are – medical health, behavioral health, housing, employment, criminal justice, school and childcare – and how when some go down, the entire net collapses, and people fall right through.
CP: Finally, what is giving you hope right now in terms of where we are at with COVID?
RW: In terms of drug use and addiction, the pandemic catapulted regulatory changes at the federal level that advocates have been clamoring for decades, and sparked much-needed momentum for further and permanent reform (like making access to addiction treatment medications much easier, supporting more mobile units and street outreach efforts, and other “low-threshold” services that meet people where they are, literally and figuratively). And though the overdose crisis isn’t dominating headlines like it was pre-COVID, many are still (or even newly) paying attention to it and recognizing it as a product of our weak social safety net, underfunded public health system, and total dearth of infrastructure and supports to help people in this county living in dire straits… many of the same issues that underlie our fragmented and deficient pandemic response. In general, I do sense a broader recognition of our collective need to be a more generous society, and to step up for the most vulnerable among us. I know this may be wishful thinking, but the hope that we will learn lessons from all of this… that’s what’s getting me through these days.
If you like what you see here and don’t already, please subscribe!