In tonight’s edition, I dive into our decline in new cases, what it means for hospitalizations and deaths, and what might be waiting for us this spring. I also dive into some vaccination metrics and share my interview with St. Louis local Julie Vomund. By necessity, she’s developed a working knowledge of how to get on vaccine waiting lists, and I am really grateful that she was willing to share her expertise with us. - Chris
COVID-19 by the Numbers
Total cases in MO: 499,272 (+7,660 from last Friday)
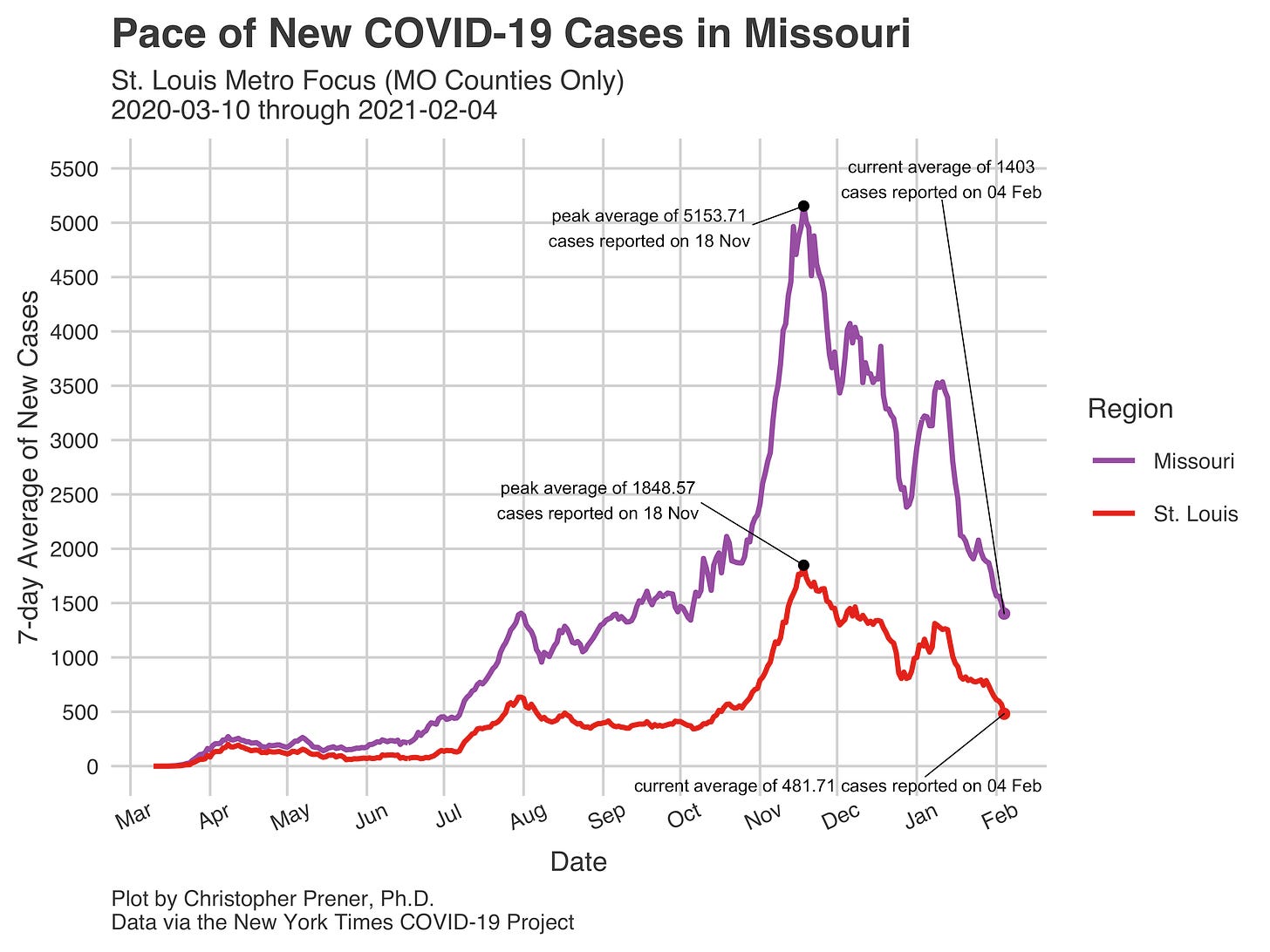
7-day average of new cases per day in MO: 1,403 (-467.71 from last Friday)
Counties with the highest per capita rates of new cases per day this past week:
Adair (47.38 per 100,000), Carroll (40.39), Harrison (40.08), Clay (37), Daviess (34.42), Joplin (34.24), Callaway (34.09), and Jasper (33.56)
Total deaths in MO: 7,518 (+356 from last Friday)
7-day average of new deaths per day in MO: 53.86 (+21 from last Friday)
These numbers are current as of Thursday, February 4th. Additional statistics, maps, and plots are available on my COVID-19 tracking site.
Summary for the Week Ending February 5th
This week's big story is the steady decline in new cases we’ve been experiencing in Missouri. Numbers have fallen dramatically over the past few weeks as we have moved past the post-holiday bump experienced in early January:
Rates have fallen in every “meso” region, each metropolitan area, and every county in Missouri. Even the counties where rates remain relatively high are seeing rates decline. This is all good news, but it is worth remembering that if rates are low in your corner of the state, they are not zero (even if, officially, almost no new cases have been reported recently). This is a critical time, with new mutations appearing just as we roll out vaccinations (more on this below). That means we need to keep up all physical distancing, masking, and handwashing behaviors we have become well-practiced with.
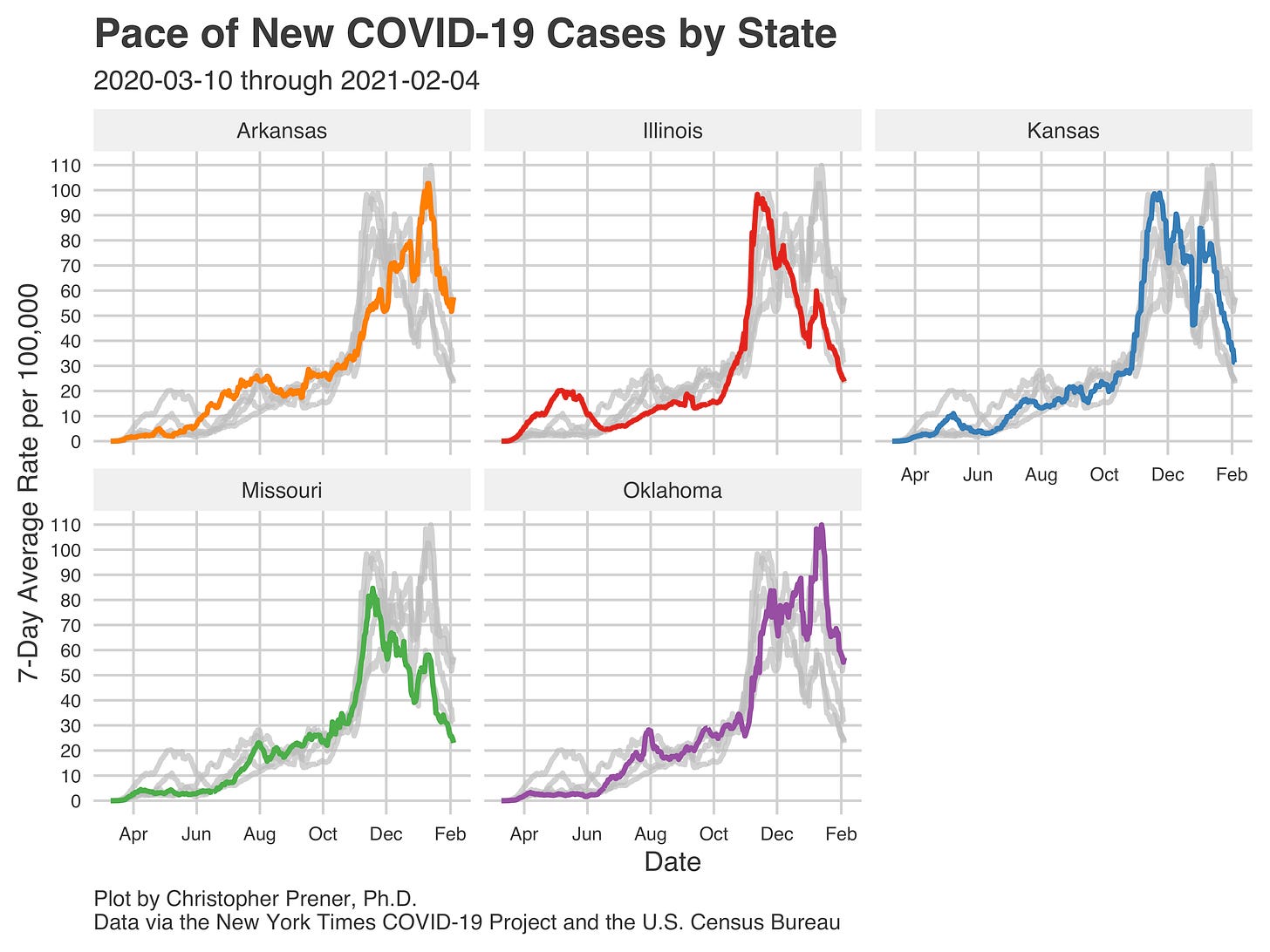
The declines in new cases may be met with skepticism, particularly because of the growing role that antigen testing plays in Missouri. I think it is good news that states reporting antigen tests in their positive counts, like Arkansas, Kansas, and Oklahoma, are all showing declines as well.
This gives me some additional evidence that what we see here in Missouri is not just an artifact from the way test results are being reported but is a genuine decline. My belief from a few weeks ago, that our number itself is artificially low but that the trend is correct, remains the same.
The real consequence of these declining rates of new cases most immediately has been with our in-patient numbers here in St. Louis. Rates of total in-patients and total ICU patients are returning to our summer and early-fall numbers. This is excellent news, especially for weary hospital staff who have been grinding for weeks under the pressure of historically high numbers of patients with COVID.
The real question hanging over my conversations with colleagues is, “what comes next?” The 1918 Influenza Pandemic had three peaks, one in the spring of 1918, one in the late fall of 1918, and one in the winter and spring of 1919. The second peak, in the fall of 1918, was the deadliest. Sound familiar? That roughly follows the shape of our in-patient numbers (see above) and our mortality data (below).
Both of these curves show just how bad our late fall in 2020 was in Missouri. So, if the 1918 Influenza Pandemic is a guide, our question right now is not if but when the third surge in cases comes, how bad it is, and how widely we can get vaccines out into the community to blunt it. Time will tell.
One point on mortality bears repeating - while hospitalizations are falling, we are still seeing deaths in Missouri higher than the prior week. Mortality lags hospitalizations, which lag new cases, so we should expect to see deaths start to decline eventually, but perhaps not yet. Again, time will tell.
Into the Weeds
The St. Louis Pandemic Task Force’s briefing today provided some important data points on vaccination progress (or lack thereof). The slide below shows how our doses are being distributed statewide right now. Of note, the majority are going to health care systems, but there are just not nearly enough of them to meet demand. The Task Force thinks about 700,000 people in Region C are eligible for the vaccine, but we are only getting 15,600 doses per week. Those doses are only about 20% of the state’s supply, even though Region C has a third of the population. We need an equitable distribution of the vaccine where no county, urban or rural, is left behind. Right now, we are a long way from that ideal.
Weekly Interview
Julie Vomund is a 15-year Hodgkin's Lymphoma survivor living in St. Louis with her husband and two dogs. She works as a paralegal for a legal nonprofit and helps clients and members of the public navigate the unfamiliar world of law and launching a business. Julie recently joined the Cancer Policy and Advocacy Team for the National Coalition for Cancer Survivorship. You can find her on Twitter tweeting about the pandemic response, living in STL, local businesses, cancer survivorship, and her dogs.
CP: You’ve been really active on Twitter speaking out about Missouri's vaccination process. What’s motivated you to pay such close attention?
JV: As a cancer survivor, I ended up with some long-term side effects from chemotherapy involving my heart and lungs but it was well-managed. I was a bit scared that week in March when everything rapidly escalated but I didn't really grow concerned until my fellow cancer survivors in the UK were contacted by their government and warned to shield in place as it was deemed unsafe for them to go out. No one in the government was reaching out to me and my doctors didn't seem to have any more guidance than I did except to confirm my risk. I was suddenly aware that I was alone in protecting myself and that I couldn't rely on the systems in place.
Once vaccine trials started, I started thinking ahead. Surely if these vaccines would be rolling out soon, we'd see RFPs from Missouri and/or the counties to plan websites and distribution...and I wasn't seeing a lot of that. I had enough time to realize that every step of the pandemic had been botched in Missouri and vaccine distribution was likely to fall into that same categorization. It made me very afraid but it inspired me to keep learning more about the process. It was a matter of life and death in my eyes.
CP: You were able to get a vaccination for yourself (which is great!). Can you share what navigating that process was like for you?
JV: I wasn't receiving any communication from my medical providers which concerned me but I wasn't surprised. I followed the advice to register at as many hospitals and local government agencies as I could. I have a lot of friends who work in healthcare in various roles so I messaged so many of them to ask how their vaccines went, how they felt about the process, if they knew their hospital's plans for connecting patients to vaccines, and if their hospital had a plan for preventing vaccine spoilage.
Several hospitals did appear to have an unofficial standby list for day-of vaccines. No one wanted to overbook appointments like an airline might, out of fear of having to turn away individuals who were high risk, but at the end of the day no one wanted to waste vaccines and they had no easy list of high-risk individuals except those that volunteered themselves. Because I had asked this question of so many individuals, my name got on at least one list and that same week I was vaccinated. Later that week I was contacted by St. Louis City for their vaccinations. I suspect the standby list practice was executed there for all the spots reserved for those of us who declined or were already vaccinated. (see the Post-Dispatch story)
CP: Stepping back from your own experience, can you reflect on both what the positives of the process were, but also what you think there is room for improvement?
JV: While I was receiving the vaccine, the elderly couple next to me were being coached on how to register for their next vaccine. They didn't know how to navigate the online system used by the hospital and no one volunteered to register them. The digital divide is going to lead to so many of our most vulnerable not receiving the vaccine. When the city emailed me for my vaccine, I had just over 12 hours to arrive for the vaccine. If I had any mobility issues or needed childcare, there's no way I could have arranged that. The lack of good communication, the lack of accessibility, and the lack of planning all leave me very concerned. This must be part of a larger conversation about what we're doing to make sure racial and ethnic disparities are being acknowledged, helping to provide disability accommodations, and also to ensure we're not excluding those who lack the ability to even drive to an administration site.
CP: You’ve been providing advice to folks on helping their loved ones or themselves get vaccinated. What are some of the things you share when you have those conversations?
JV: So many people reaching out to me are sharing how scared they are for elderly or sick parents. I'm experiencing this myself and my relative still isn't vaccinated. I try to let them know that just because someone hasn't gotten the vaccine doesn't mean they themselves have failed. Our systems failed us. There's a lot of guilt associated with the process of getting prioritized for the vaccine over someone else or in feeling like we can't protect family so it's important to know you aren't alone in feeling guilt but you don't have to hold onto that emotion.
I also try to explain the infrastructure in place. A lot of people really aren't familiar with hospitals or government so I think this entire process is very new to them. First, know your phase and tier. Register everywhere; if you own hunting ground in another county, register there too. We just heard today (Monday) that hospitals will now be receiving 53% of the vaccines and only 8% to Departments of Health so at this point I'd urge everyone to register with any and every hospital but if you are high risk, reach out to any provider you've had contact with in the last 24 months and specifically nudge them about high-risk conditions they might not know you have because they aren't your specialist. The unofficial standby lists are likely to become official so this is the time to even review old medical payments just to make sure you didn't forget any providers. This of course assumes you have a provider and so many don't. For those individuals, we've just learned 23% of vaccines will be going to National Guard sites. These will likely be coordinating with departments of health so be sure you are following social media for them as it is often updated well before a webpage. The state hasn't yet coordinated registrations for those and often the only way is through a local social media page.
Like I mentioned before, many seniors aren't comfortable registering with 4 hospital websites. They might only check their email twice a week and would miss an email Friday night for a Saturday morning vaccine. For adults with bandwidth to help senior parents, register them with accounts. Get permission to register them online with a shared email address or have their email forwarded to you. Empower your parents to ask for accomodations from hospitals that insist they must register online. Be polite but firm. And while you wait, stay safe. Help is around the corner so don't let your guard down now.
CP: Finally, what is giving you hope right now in terms of COVID-19?
JV: Because I have so many family and friends in healthcare, I'm seeing them vaccinated and I've found myself vaccinated. It fills me with joy to know that we are growing safer by the day and that we're in a (hopefully longer-term) decline of spread. I can't overstate how at risk I was of dying if I was diagnosed with this and the level of protection I'll soon have doesn't mean I'll be changing my behaviors but it means maybe I can afford to retire from my unofficial pandemic monitoring program.