This week’s edition is full of updates on the antigen case count releases, recent trends in cases, and vaccinations in Missouri. I’m also sharing new updates to my COVID-19 tracking site as well as perspectives on where we’ve been in the past year and where we’re going from friends-of-the-newsletter Julie Vomund and Fred Buckhold, MD. Finally, I have an excellent interview with Hilary Reno, MD, Ph.D., on how the pandemic has affected our ability to identify and treat sexually transmitted infections. - Chris
COVID-19 by the Numbers
Total cases in MO: 576,363 (+2,612 from last Thursday)
7-day average of new cases per day in MO: 602.14
Counties with the highest per capita rates (per 1,000) of new cases per day this past week:
Montgomery (44.55 per 100,000), Gasconade (29.06), Carter (23.05), Crawford (21.77), Macon (21.54), Mississippi (20.78), St. Clair (19.79), and Schuyler (19.04)
Total deaths in MO: 8,806 (+54 from last Thursday)
7-day average of new deaths per day in MO: 11.14 (-10.71 from last Thursday)
Percent of people initiating vaccination: 21%
Percent of people completing vaccination: 11%
Case and mortality numbers are current as of Wednesday, March 17th. Vaccination numbers are current as of Thursday, March 18th. Additional statistics, maps, and plots are available on my COVID-19 tracking site.
New on the Tracking Site
My tracking site now contains several new and updated data sources:
There is now a vaccination page on the site with statewide maps and per capita vaccination rates by district.
The home page includes a vaccine progress tracking plot.
The disparities page now includes data on racial and ethnic disparities in initiated vaccinations.
The Kansas City ZIP Code map has received an overhaul that brings the case totals up-to-date after several underlying data sources were moved to new locations.
Illness Trends in the Past Week
After last week’s large dump of antigen test results, I spent almost a week overhauling the plots available on the tracking site. On Tuesday, we got our first look at 7-day averages that included antigen test results by county but did not include the initial large dump of cases the week prior. You can see how antigen tests biased our trends in December, January, and February downward at the state level. When antigen tests started to become increasingly common at the beginning of December, Missouri and Illinois had similar cumulative rates. As December and January progressed, Missouri’s trend increased at a slower rate before snapping back up to be even with Illinois on March 8th once antigen tests were factored in.
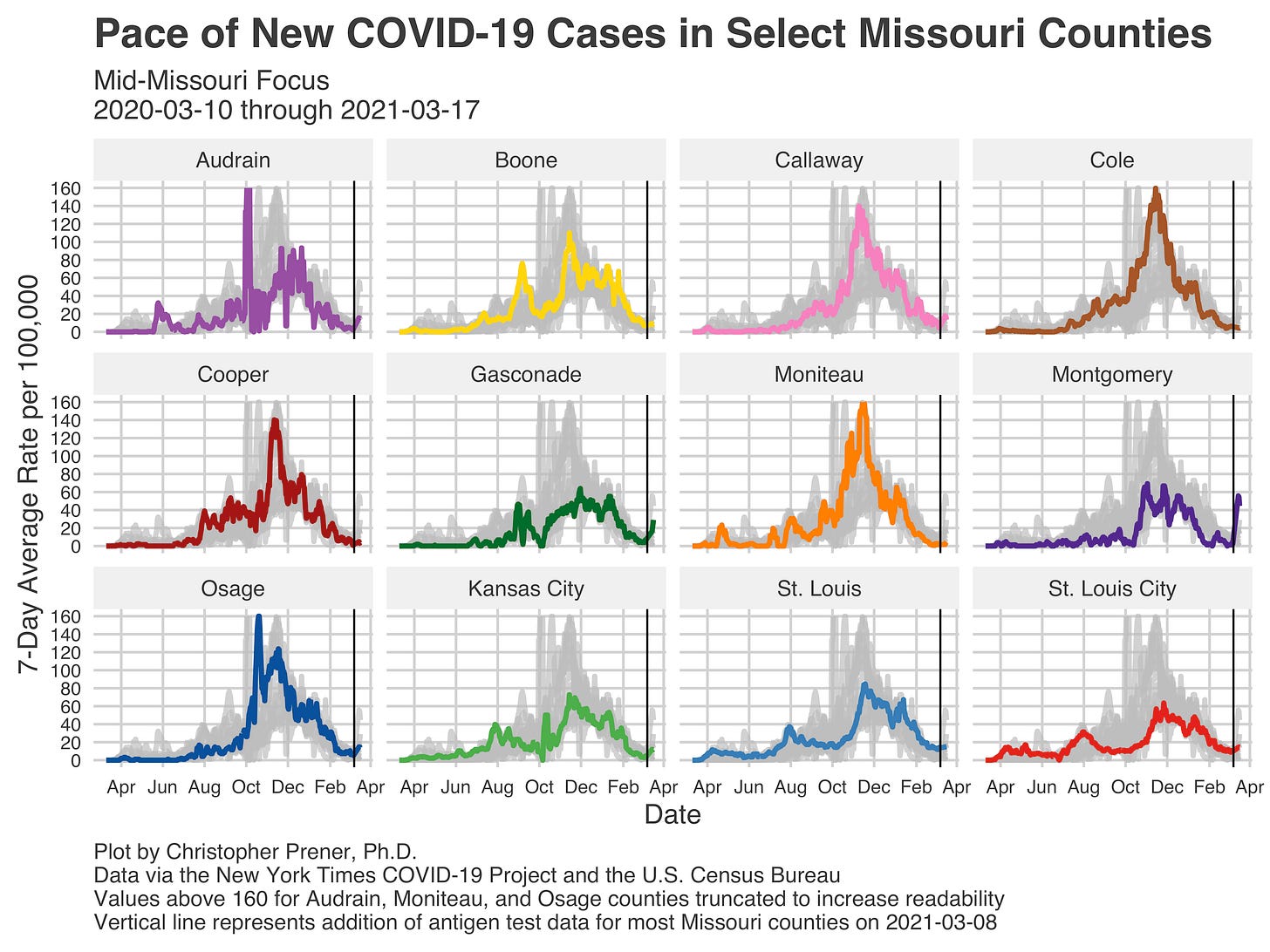
Despite the inclusion of antigen tests, our cases statewide remain quite low. Rates spring up statewide after March 8th by a hundred or so per day. This was not even across the state, however. St. Louis, for example, saw little change on the plot below because both the City and the County were already disclosing antigen tests in their daily counts, and my data provider, the New York Times, was capturing those counts directly.
In other parts of the state, however, there were significant jumps. Take Southwest Missouri, for example, where counties like Jasper, Newton, and Barry all saw their cumulative cases shift upward in significant ways after the antigen tests were reported.
Notice, however, that rates did not change in McDonald and Dade counties, which likely did not have large numbers of antigen tests to administer compared to surrounding counties.
There are a small number of counties that are seeing upticks in new cases, none more significant than Montgomery County, whose seven-day average jumped to nearly sixty before declining yesterday to the mid-forties.
Vaccination Trends in the Past Week
We are starting to see positive movement in recent vaccinations towards both Kansas City (District A) and St. Louis (District C). Over the last week, both Districts have seen administration rates grow, and they are now receiving vaccinations at the highest rate in Missouri.
That is positive news, given the dearth of vaccines we had seen over February. However, when we look at the initiated vaccinations overall, St. Louis, in particular, has a middling rate of initiated vaccinations (meaning the number of people with at least one dose of the Moderna and Pfizer vaccines received or having received the Johnson & Johnson vaccination).
There are large events planned in both St. Louis and Kansas City in the next few days to push these rates forward. The goal here is not for St. Louis and Kansas City to have the highest rates but rather to deal with the imbalance between events in some rural counties where appointments go unfilled while waiting lists are very long in Missouri’s two largest cities.
Looking Backward
Last week, several folks who have sat down at their keyboards for interviews returned to share the moment when the pandemic became real for them around a year ago. Tonight, I am excited to share another reflection on that moment.
Fred Buckhold, MD, Saint Louis University School of Medicine and SSM Saint Louis University Hospital (Interview)
My worry started that first week of March. That was when I realized (and I can't exactly remember how) that this was going to hit us like a tsunami. As I run a residency program of 84 resident physicians, I sent an email on 3/2 advising them to reconsider travel plans and cancel if they could, fearing that things would be shutting down. That first few days, I took so much heat. By the end of the week, things started shutting down. The second thing that sticks out was when my first resident became ill. At that time, we were so short of equipment, and I had this perpetual fear that someone would get seriously ill. Having that conversation with their parents in my head and worrying whether we did enough to protect our people - that weighed heavily on me. I'll never forget that feeling. Fortunately, although many of our residents got sick (mostly from community spread), none were hospitalized. I'm very grateful for that.
Looking Forward
In addition to this look backward, I also wanted to share perspectives on the things we need to remember as we move into year two of COVID. While we are already seeing some signs of hope in lower current case rates and increasing vaccination progress, I feel strongly that we cannot forget the incredible stress we placed on health care providers or the health disparities in morbidity and mortality we have experienced.
Julie Vomund (Interview)
Pre-pandemic, the disabled community was regularly told that accommodations couldn't be made for them. Then when March hit, things like curbside access, work from home, and other accommodations began almost immediately. It became possible because the able-bodied needed them. When the pandemic went on longer than some expected, the tone shifted to how only the disabled needed to stay home and mask while the able-bodied should be able to move on with their lives. So many people didn't blink when the pandemic killed our elderly and disabled neighbors as if they were a sacrifice to get us "back to normal" and not something tragic that could have been prevented. The disabled community has a right to be safe and accommodated, and we must address the failures to ensure this when disabled individuals were at their most vulnerable.
Fred Buckhold, MD, Saint Louis University School of Medicine and SSM Saint Louis University Hospital (Interview)
I do not want to forget that so many healthcare workers were left on an island, without proper equipment, and stepped up and did a job. There are so many holes in our healthcare. These holes cost our society, whether it be with health outcomes or financial cost. We depended on the pride, professionalism, and altruism of many doctors, nurses, and other professionals, and those resources are at risk of depletion. We also need to address the massive racial and socioeconomic disparities in health outcomes, which were laid bare in this pandemic (and in determining who gets vaccines).
Weekly Interview
Hilary Reno, MD, Ph.D., is an Associate Professor in Medicine at Washington University, focused on sexual health care. She has been the medical director of the St. Louis County Sexual Health clinic for thirteen years. In addition, Dr. Reno is a medical consultant with the CDC, Division of STD Prevention, and a co-author of the 2021 CDC STI Treatment Guidelines. She also directs the St. Louis STI/ HIV Prevention Training Center.
CP: Can you start by telling us a little bit about where things stood with sexually transmitted infections (STIs) before the pandemic?
HR: STIs are a leading public health threat in the world, the US, and the St. Louis Region. Rates of all STIs have increased markedly since 2014, especially gonorrhea (63% increase) and syphilis (71% increase). In addition, marked racial disparities exist, with the rate of gonorrhea being nineteen times greater in Black Americans compared to white Americans in St. Louis County (2018 data). Pre-pandemic, the sexual health of the US and St. Louis was not good.
In St. Louis, though there are many clinics and organizations that offer STI and HIV testing at no or low cost, enrollment or demonstration of income requirements may be needed and act as a barrier. Certainly, the stigma of seeking sexual health care is its own barrier. Add on to these barriers the lack of insurance, the difficulty youth have accessing confidential care, and the lack of comprehensive sexual health education and one can understand the complexities of STIs in the St. Louis region even before the pandemic.
CP: Wow. I had no idea that rates had climbed as much as they have. Since COVID-19 and the lockdown, how have these rates changed?
HR: We know that to be open and operate during the pandemic, clinics needed PPE (masks, eyewear at least) to operate and some closed to clinical care initially. In state and local health departments, staff were re-assigned to COVID contract tracing and planning, necessitating the closure of some health department-based STI clinics. I direct STIRR, the St. Louis STI Regional Response Coalition (established in 2015), and we have a list of all STI/ HIV testing sites and their operating hours. We surveyed the sites in April 2020 and November 2020 during the first and third (?) wave of COVID in the St. Louis region.
Our findings are pending publication, but we found that during April 2020, only 7% of clinics on our list remained fully open without any changes to services. By November 2020, that percentage had increased to 29. We found that only 6% of clinics in high prevalence zip codes for chlamydia remained fully operational, and 14% in medium prevalence zip codes. At that time, 5% of clinics remained closed, 29% were open (had returned to pre-pandemic services), 55% were modified in their services offered, and 11% were unknown status. So we have additional barriers to sexual health that are directly COVID related.
Also, there is evidence nationally that decreased STI and HIV testing was occurring during 2020; this is based on data from large commercial labs. Regionally, we looked at BJC data (15 hospitals, over 100 primary care clinics) and found the following from Jan 2020 through July 2020:
a decrease of 45% in testing for gonorrhea and chlamydia
a decrease of 43% in testing for HIV.
The decreased volume of testing for gonorrhea/ chlamydia as well as HIV was seen across age, race, and gender groups as well as in various clinical settings. The good news is that testing at BJC has largely returned to pre-COVID volumes. Over the 10-week period of decreased testing with the first stay-at-home orders, calculations indicate that 5000 tests for HIV and 4500 tests for gonorrhea/chlamydia were missed. We are concerned that cases have not declined, they have just not been identified.
Unfortunately, the St. Louis County Sexual Health Clinic is seeing two-thirds the volume of patients compared to pre-pandemic volume. There were testing kit shortages in the fall and winter of 2020 as companies devoted manufacturing to COVID testing supplies. For a short amount of time, we were not able to offer gonorrhea/ chlamydia testing to everyone because of these shortages. However, the clinic never fully closed to patients, and the clinic staff should be commended for continuing to offer testing and treatment during the pandemic. It was not always easy.
Luckily, testing kit availability is increasing. We are still challenged by the need to space out patients with appointments as well as fewer chairs in the waiting area. This decreases how many patients we can see. Luckily, PPE is in good supply, and rates of COVID are decreasing. Hopefully, as more people get the vaccine, they will be able to attend to their regular medical care, which includes sexual health care.
CP: From a policy standpoint, has COVID-19 changed how you think we should be addressing public health work, especially around STIs, in Missouri?
Missouri does not fund STI treatment or care (except for some funds for the state public health lab that starting in the last 2 years). All funding comes from the federal government. Missouri has the lowest dollar per person funding for public health of all states, and so funding for STI and HIV testing and prevention is from the Federal government and local public health departments. I think the questions are, has COVID-19’s impact on health care and health care workers, have the deaths from one virus, or have the health care disparities and racism laid bare by the pandemic raised the need to fund public health to something that our state politicians will act on. Some states are increasing public health funding secondary to the experience of the pandemic. Given the environment of Missouri, I do not think we will see that effort here. Therefore, we are left with improving the public health system we have and working to obtain funding from the Federal government and foundations.
We must be innovative. We need to focus on cooperation. We should be using data to improve services and programs. For example, the End the HIV Epidemic initiative has provided some increased funding, some of which is focused on traditional STI clinics. The St. Louis County Sexual Health clinic is one of seven clinics in the US to receive a 5-year grant to improve HIV prevention work at the clinic. This grant will improve infrastructure and support the expansion of our STI/ HIV prevention services. The funding also supports the development of a Regional Sexual Health data platform that will allow us to visualized data on STI testing like never before—though cooperative work in St. Louis with COVID laid some of the groundwork. The data can be used throughout the region for program evaluation to focus resources for those that need it the most. Data on testing and management on such a large scale for the region will move us towards health equity. I am thrilled the HHS/ CDC recognized that this effort is worth the investment.
CP: Congratulations on the grant - that is really exciting! Beyond being able to help move the work of the St. Louis County Sexual Health Clinic forward, what is giving you hope right now in terms of where we are at with COVID?
HR: The efficacy of all vaccines is greater than we were hoping for. And though the supply of vaccines is increasing, the issue is mobilizing to get those vaccines distributed equitably and then into arms. In the interest of equity, people of color should be able to receive the vaccine at a younger age, and vaccination clinics should be in neighborhoods hardest hit by COVID-19. I have volunteered at several vaccination clinics, and there are filled with joy and support for those who are getting vaccinated. We also need to be concerned about the global vaccination effort. Countries need to advocate and move to support global vaccination because other variants will evolve that could be challenging. Many are calling for a People’s Vaccine because, as we are often reminded, when an infectious disease affects one country, we are all affected.
If you like what you see here and don’t already, please subscribe!